Acute mediastinitis in a third-level public hospital in Bogotá city, Colombia: a 6-year retrospective series.
Mediastinitis aguda en un Hospital público de tercer nivel en la ciudad Bogotá, Colombia: Serie retrospectiva de 6 años.

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Ninguna publicación, nacional o extranjera, podrá reproducir ni traducir sus artículos ni sus resúmenes sin previa autorización escrita del editor; sin embargo los usuarios pueden descargar la información contenida en ella, pero deben darle atribución o reconocimiento de propiedad intelectual, deben usarlo tal como está, sin derivación alguna.
Show authors biography
Introduction. Acute mediastinitis is an underdiagnosed entity with diverse clinical results, in addition to having multiple etiologies, among which are post-cardiac surgery, being the most studied and with clearer statistics, others less analyzed such as those caused by esophageal perforation and descending necrotizing mediastinitis, traumatic and idiopathic diseases. We describe the paraclinical findings, management, and prognosis of this entity in a third-level public hospital in the city of Bogotá, Colombia, where specialties such as thoracic surgery, pneumology, and gastroenterology are available.
Materials and methods. We conducted a descriptive observational study with a retrospective search of the medical records of patients diagnosed with acute mediastinitis and related (we ruled out complications from cardiac surgery as an exclusion criterion); Paraclinical variables, etiologies, type of image, microbiology, management, complications, and mortality were described in this group of patients.
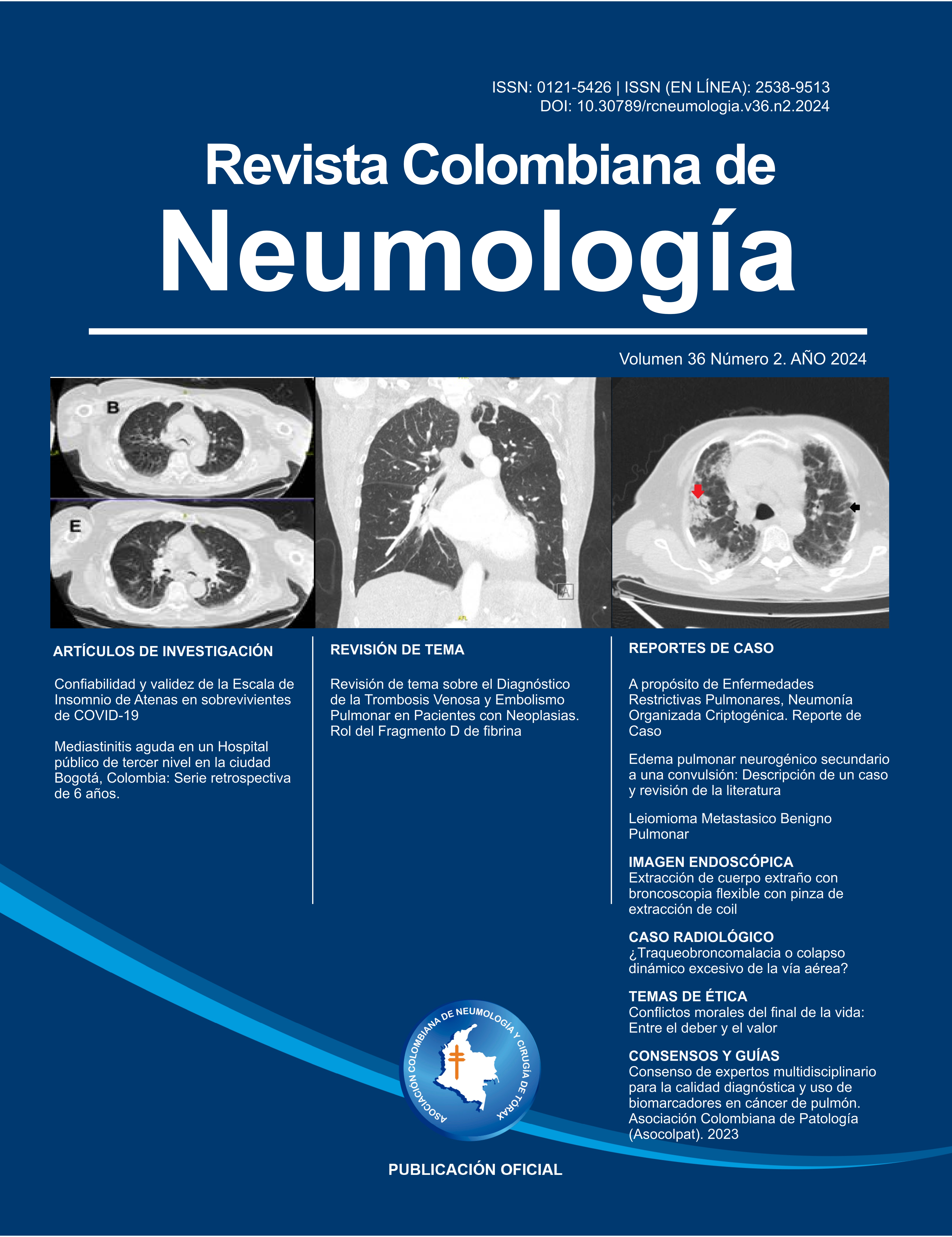
Results. 35 subjects in a period of 6 years, the majority were men in 82.9% with an average age of 44 years, the most frequent etiologies were esophageal perforation (PE) with 48.7% (the main cause was foreign body ingestion) and descending necrotizing mediastinitis (DNM) with 45.7% (main trigger was odontogenic abscess with 62.5%); drug dependence was the most frequent comorbidity in 48%; the most frequently performed imagen study was computed tomography in 94.3%, mediastinal edema and emphysema were the main radiological findings, gram-negative bacilli and gram-positive cocci the most found in cultures, surgery being the main management, distributed between cervicotomy and thoracoscopy (VATS) depending on the etiology; overall mortality was 22.9% and the average hospital stay was about 29 days.
Discussions and conclusions. This is one of the largest Colombian studies on this pathology. Because it is performed in a public hospital, various etiologies are obtained. Drug dependence as a prevalent comorbidity associated with poor oral hygiene, it generates odontogenic septic foci as the origin of descending mediastinitis and ingestion of foreign bodies in esophageal perforation with mediastinitis; These findings differ from what has been reported in the world literature, given that by not having an endoscopic intervention service, iatrogenesis was less frequent. Training and skills in minimally invasive management or a multidisciplinary conservative approach have displaced major surgeries performed in the past, our data on hospital stay and mortality are within the range described in world literature.
Article visits 287 | PDF visits 345
Downloads
- Athanassiadi KA. Infections of the Mediastinum. Thorac Surg Clin [Internet]. 2009;19(1):37–45. doi: 10.1016/j.thorsurg.2008.09.012
- Macrí P, Jiménez MF, Novoa N, Varela G. Análisis descriptivo de una serie de casos diagnosticados de mediastinitis aguda. Arch Bronconeumol [Internet]. 2003;39(9):428–30. doi: 10.1016/S0300-2896(03)75419-2
- Chen LF, Arduino JM, Sheng S, Muhlbaier LH, Kanafani ZA, Harris AD, et al. Epidemiology and outcome of major postoperative infections following cardiac surgery: Risk factors and impact of pathogen type. Am J Infect Control. 2012 Dec;40(10):963–8. doi: 10.1016/j.ajic.2012.01.012
- González-García R, Risco-Rojas R, Román-Romero L, Moreno-García C, López García C. Descending necrotizing mediastinitis following dental extraction. Radiological features and surgical treatment considerations. J Cranio-Maxillofacial Surg [Internet]. 2011;39(5):335–9. doi: 10.1016/j.jcms.2010.10.001
- Vidarsdottir H, Blondal S, Alfredsson H, Geirsson A, Gudbjartsson T. Oesophageal perforations in Iceland: A whole population study on incidence, aetiology and surgical outcome. Thorac Cardiovasc Surg. 2010;58(8):476–80. DOI: 10.1055/s-0030-1250347
- Giraldo Montoya Á, Ucros E, Varón F, Mugnier J. Dolor torácico más allá de un síndrome coronario. Rev Médica Risaralda. 2015;21(1):68–72. ISSN 0122-0667.
- Martínez Vallina P, Espinosa Jiménez D, Pérez LH, Triviño Ramírez A. Mediastinitis. Arch Bronconeumol. 2011;47(SUPPL. 8):32–6. https://doi.org/10.1016/S0300-2896(11)70065-5.
- Arantes V, Campolina C, Valerio SH, De Sa RN, Toledo C, Ferrari TA, et al. Flexible esophagoscopy as a diagnostic tool for traumatic esophageal injuries. J Trauma - Inj Infect Crit Care. 2009;66(6):1677–82. DOI: 10.1097/TA.0b013e31818c1564.
- Rajaram R, Decamp MM. Chapter 157: Acute and Chronic Mediastinal Infections. In: LoCicero J, Feins Richard H, Colson Y, L.Rocco G, editors. Shields' General Thoracic Surgery. 8th editio. Two Commerce Square, 2001 Market Street, Philadelphia, PA 19103: Lippincott Williams & Wilkins; 2019.
- Estrera AS, Landay MJ, Grisham JM, Sinn DP, Platt MR. Descending necrotizing mediastinitis. Surgery, Gynecol & Obstet [Internet]. 1983;157(6):545–52. Available from: http://europepmc.org/abstract/MED/6648776. PMID: 6648776
- Zelada I, Farina C, Lee C, Agüero Á. Acute Mediastinitis. Retrospective Analysis of 12 Cases. Cir Paraguaya. 2019;43(1):12–5. https://doi.org/10.18004/sopaci.2019.abril.12-15
- Vásquez Julio C, Montesinos Efraín, Castillo Luis, Rojas Luis, Peralta Julio. Perforación esofágica y Mediastinitis por ingestión de espina de pescado: Reporte de 3 casos. Rev. gastroenterol. Perú [Internet]. octubre de 2006 [citado el 18 de julio de 2023]; 26(4): 400-403. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292006000400010&lng=es.
- Cunha Fatureto M, Alves Das Neves-junior M, Cunha Santana T DE. Acute mediastinitis. Restropective analysis of 21 cases*. J Bras Pneumol. 2005;31(4):307–18. https://doi.org/10.1590/S1806-37132005000400007
- Marty-Ane CH, Alauzen M, Alric P, Serres-Cousine O, Mary H, Marty-Ané CH, et al. Descending necrotizing mediastinitis: Advantage of mediastinal drainage with thoracotomy. Ann Thorac Surg. 1994;68(1):212–7. https://doi.org/10.1016/S0022-5223(94)70453-8
- Marty-Ané CH, Berthet JP, Alric P, Pegis JD, Rouvière P, Mary H. Management of descending necrotizing mediastinitis: An aggressive treatment for an aggressive disease. Ann Thorac Surg. 1999;68(1):212–7. https://doi.org/10.1016/S0003-4975(99)00453-1.
- Nguyen DC, Pham VT, Pham HB, Pham LC NM. Surgical management of mediastinitis and mediastinal abscess: a series of 56 cases. Ann Chir 2003; 128 570-571. 2003;128:570–1. DOI: 10.1016/j.anchir.2003.07.001
- M A Rubio, J J Rubio, M A Ospitia JFS, R Medina WFB. Complicaciones Asociadas Al Trauma Penetrante de Esófago, Experiencia De 11 Años En El Hospital Universitario de Neiva. Panam J Trauma, Crit Care Emerg Surg. 2017;6(1):30–4. DOI: 10.5005/jp-journals-10030-1168.
- Karkas A, Chahine K, Schmerber S, Brichon P, Righini CA. Optimal treatment of cervical necrotizing fasciitis associated with descending necrotizing mediastinitis. 2010;(January 1995):609–15. https://doi.org/10.1002/bjs.6935.
- Robles-Pérez E, Córdova-López JL, López-Rodríguez R, et al. Factores que inciden en la mortalidad de la mediastinitis aguda necrosante descendente. Rev Hosp Jua Mex. 2018;85(3):127-135.
- Héctor Jairo Umaña, Diego Medina DL. Semiología del dolor torácico en patologías potencialmente fatales. Rev Médica Risaralda. 2011;17(2):113–23. DOI: https://doi.org/10.22517/25395203.7599.
- Gómez Zuleta M, Rodríguez Gómez A, Siado A. Hematoma esofágico intramural: de la disección a la perforación (AU) TT - Intramural esophageal hematoma: dissection of the perforation. Rev colomb gastroenterol [Internet]. 2012;27(2):125–33. Available from: http://www.scielo.org.co/scielo.php?script=sci_arttext&%0Apid=S0120-99572012000200012&%0Alng=es&%0Anrm=iso&%0Atlng=es%0Atlng=en. ISSN (Versión impresa): 0120-9957.
- Garzón D, Barragán F, Martin D, Avila Y, Ali A. Perforación esofágica y fístula esofagopleural por Candida albicans: reporte de un caso. Acta Colomb Cuid Intensivo [Internet]. 2016;16(4):290–3. Available from: http://dx.doi.org/10.1016/j.acci.2016.06.002
- Benítez E, Alfonso M, Lesmes MC, Barón V, Hernández Ó, Oliveros G. Perforación aorto-esofágica, diagnóstico clínico e imaginológico: reporte de dos casos clínicos con manejo endovascular. Rev Colomb Cirugía. 2019;34(2):190–8. https://doi.org/10.30944/20117582.114.
- Nazario DAM, Suárez RJA, Castilla CG, et al. Caracterización clínica, diagnóstica y quirúrgica de pacientes con mediastinitis aguda por perforación esofágica cervical y torácica. MediSan. 2017;21 (11):3152-3162.
- Gómez Zuleta Martín Alonso, Viveros Carreño David Andrés, Buitrago Melissa. Síndrome de Boerhaave: a propósito de dos casos. Rev Col Gastroenterol [Internet]. junio de 2014 [citado el 18 de julio de 2023]; 29(2): 179-182. Disponible en: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-99572014000200014&lng=en.26. M Hernández-Sómerson LO-S. Síndrome de Boerhaave : relato de caso Boerhaave ´ s syndrome : case report. Acta Med Colomb. 2018;Vol. 43 No(1):83–4.
- Piedrahita Botero MA, Berrouet Mejía MC. Síndrome de Boerhaave como complicación del consumo de alcohol: reporte de caso. Med UPB [Internet]. 3 de marzo de 2021 [citado 19 de julio de 2023];40(1):77-81. Disponible en: https://revistas.upb.edu.co/index.php/medicina/article/view/7021 DOI: https://doi.org/10.18566/medupb.v40n1.a10
- Rockbrand Campos LP, Koutsowris Sáenz S, Rojas Carranza HV. Síndrome de Boerhaave: manejo mínimamente invasivo. Rev.méd.sinerg. [Internet]. 1 de septiembre de 2019 [citado 18 de julio de 2023];4(9):e273. Disponible en: https://revistamedicasinergia.com/index.php/rms/article/view/27329. https://doi.org/10.31434/rms.v4i9.273.
- Pérez-orbegozo MA, Buitrago-trujillo AP, Fernández GN, Lora-aguirre A, Suárez-olarte LM, Orrego-colorado JA, et al. Mediastinitis necrotizante descendente de origen odontogénico Descending necrotizing mediastinitis of odontogenic origin. Acta Otorrinolaringol Cirugía Cabeza y Cuello [Internet]. 2021;49(3):230–6. Available from: DOI.10.37076/acorl.v49i3.6404
- Andrés Leonardo Fuentes F.*, Luis Felipe Romero M.*, María Paula Olivera A.* JACL, A.* HAU. Mediastinitis descendente en el contexto de la angina de Ludwig. Artículo de revisión. Acta Otorrinolaringol Cirugía Cabeza y Cuello [Internet]. 2022;50(2):150–8. Available from: DOI.10.37076/acorl.v50i2.612
- Quintana JC, Pinilla González R, González Rivera A, López Lazo S, Rodríguez Vásquez B. Shock séptico en una embarazada post extracción dental. Presentación de un caso. Acta Odontol. Colomb. [Internet]. 1 de enero de 2016 [citado 18 de julio de 2023];6(1):177-86. Disponible en: https://revistas.unal.edu.co/index.php/actaodontocol/article/view/58858 DOI:10.15446/aoc
- Carrott PW, Low DE. Advances in the Management of Esophageal Perforation. Thorac Surg Clin. 2011;21(4):541–55. DOI: https://doi.org/10.1016/j.thorsurg.2011.08.002
- Pastene B, Cassir N, Tankel J, Einav S, Fournier PE, Thomas P, et al. Mediastinitis in the intensive care unit patient: a narrative review. Clin Microbiol Infect [Internet]. 2020;26(1):26–34. Available from: https://doi.org/10.1016/j.cmi.2019.07.005
- Kimura, A., Miyamoto, S. and Yamashita, T. (2020), Clinical predictors of descending necrotizing mediastinitis after deep neck infections. The Laryngoscope, 130: E567-E572. https://doi.org/10.1002/lary.28406
- Makeieff, M., Gresillon, N., Berthet, J.P., Garrel, R., Crampette, L., Marty-Ane, C. and Guerrier, B. (2004), Management of Descending Necrotizing Mediastinitis. The Laryngoscope, 114: 772-775. https://doi.org/10.1097/00005537-200404000-00035.
- Sugio K, Okamoto T, Maniwa Y, Toh Y, Okada M, Yamashita T, et al. Descending necrotizing mediastinitis and the proposal of a new classification. JTCVS Open [Internet]. 2021;8(C):633–47. Available from: https://doi.org/10.1016/j.xjon.2021.08.001
- Ridder, Gerd J. MD * ; Maier, Wolfgang MD * ; Kinzer, Susanne MD * ; Teszler, Christian B. MD *† ; Boedeker, Carsten C. MD * ; Pfeiffer, Jens MD *. Mediastinitis Necrotizante Descendente: Tendencias contemporáneas en etiología, diagnóstico, manejo y resultado. Annals of Surgery 251(3):p 528-534, marzo de 2010. | DOI: 10.1097/SLA.0b013e3181c1b0d1
- Esther Papalia et. al, Descending necrotizing mediastinitis: surgical management, European Journal of Cardio-Thoracic Surgery, Volume 20, Issue 4, October 2001, Pages 739–742, https://doi.org/10.1016/S1010-7940(01)00790-4
- Martin RF. Descending necrotising mediastinitis: a case report and review of the literature. Vol. 9, Eur J Cardio-thorac Surg (1995) 9:161-162. 1995. p. xiii–xiv. https://doi.org/10.1016/S1010-7940(05)80067-3
- Swinnen J, Eisendrath P, Rigaux J, Kahegeshe L, Lemmers A, Le Moine O, et al. Self-expandable metal stents for the treatment of benign upper GI leaks and perforations. Gastrointest Endosc [Internet]. 2011;73(5):890–9. doi: 10.1016/j.gie.2010.12.019
- C Akman, F Kantarci, S Cetinkaya, Imaging in mediastinitis: a systematic review based on aetiology, Clinical Radiology, Volume 59, Issue 7, 2004, Pages 573-585, ISSN 0009-9260, https://doi.org/10.1016/j.crad.2003.12.001. (https://www.sciencedirect.com/science/article/pii/S0009926004000029)
- Qu L, Liang X, Jiang B, Qian W. Risk Factors Affecting the Prognosis of Descending Necrotizing Mediastinitis From Odontogenic Infection. J Oral Maxillofac Surg [Internet]. 2018;76(6):1207–15. doi: 10.1016/j.joms.2017.12.007
- Wheatley MJ, Stirling MC, Kirsh MM, Gago O, Orringer MB. Descending necrotizing mediastinitis: Transcervical drainage is not enough. Ann Thorac Surg [Internet]. 1990;49(5):780–4. doi: 10.1016/0003-4975(90)90022-X
- Gradica F, Argjiri D, Cani, Kokici F, Vyshka A, Dogjani A, et al. Surgical management of descendent necrotizing mediastinitis by cervicostomy. Eur J Surg Oncol [Internet]. 2019;45(2):e87. doi: 10.1016/j.ejso.2018.10.310
- Corsten MJ, Shamji FM, Odell PF, et alOptimal treatment of descending necrotising mediastinitis.Thorax 1997;52:702-708. http://dx.doi.org/10.1136/thx.52.8.702
- Endo, S., Murayama, F., Hasegawa, T. et al. Guideline of surgical management based on diffusion of descending necrotizing mediastinitis. Jpn J Thorac Caridovasc Surg 47, 14–19 (1999). https://doi.org/10.1007/BF03217934
- Yano M, Numanami H, Akiyama T, Taguchi R, Furuta C, Ogawa T, Kishimoto M, Okamoto H, Inukai D, Haniuda M. Distribution of descending necrotizing mediastinitis and efficacy of distribution-specific drainage. J Thorac Dis. 2020 May;12(5):2380-2387. doi: 10.21037/jtd.2020.03.82. PMID: 32642143; PMCID: PMC7330360.
- Gomez-Esquivel, R., Raju, G.S. Endoscopic Closure of Acute Esophageal Perforations. Curr Gastroenterol Rep 15, 321 (2013). https://doi.org/10.1007/s11894-013-0321-9.
- Jones WG, Ginsberg RJ. Esophageal perforation: A continuing challenge. Ann Thorac Surg [Internet]. 1992;53(3):534–43. Available from: http://dx.doi.org/10.1016/0003-4975(92)90294-E
- Huber-Lang, M., Henne-Bruns, D., Schmitz, B. et al. Esophageal Perforation: Principles of Diagnosis and Surgical Management. Surg Today 36, 332–340 (2006). https://doi.org/10.1007/s00595-005-3158-5
- Atilla Eroǧlu et al, Esophageal perforation: the importance of early diagnosis and primary repair, Diseases of the Esophagus, Volume 17, Issue 1, 1 June 2004, Pages 91–94, https://doi.org/10.1111/j.1442-2050.2004.00382.x
- Port JL, Kent MS, Korst RJ, Bacchetta M, Altorki NK. Thoracic esophageal perforations: A decade of experience. Ann Thorac Surg. 2003;75(4):1071–4. https://doi.org/10.1016/S0003-4975(02)04650-7.
- Yuasa N, Hattori T, Kobayashi Y, Miyata K, Hayashi Y, Seko H. Treatment of spontaneous esophageal rupture with a covered self- expanding metal stent. Gastrointest Endosc. 1999;49(6):777–80. DOI:https://doi.org/10.1016/S0016-5107(99)70300-7
- D. Mathieu et al, Cervical Necrotizing Fasciitis: Clinical Manifestations and Management, Clinical Infectious Diseases, Volume 21, Issue 1, July 1995, Pages 51–56, https://doi.org/10.1093/clinids/21.1.51
- Hector M. Prado–Calleros, MD, Edgardo Jimenez–Fuentes, MD IJ. Descending necrotizing mediastinitis: Systematic review on its treatment in the last 6 years, 75 years after its description. Head Neck [Internet]. 2016;38:E2275–E2283. Available from: DOI 10.1002/hed.24183