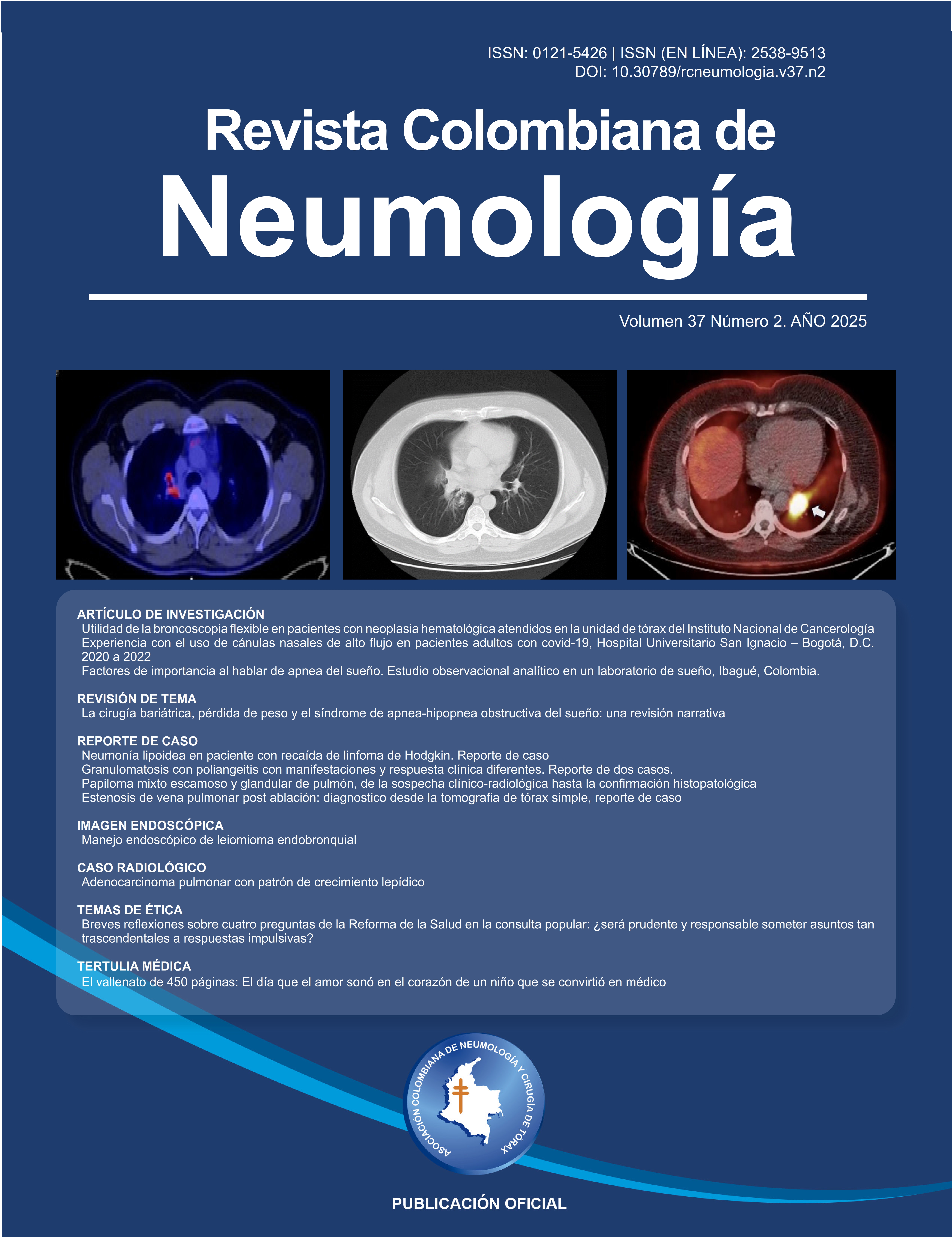
Key factors associated with sleep apnea: An analytical observational study conducted in a sleep laboratory in Ibagué, Colombia.
Factores de importancia al hablar de apnea del sueño. Estudio observacional analítico en un laboratorio de sueño en Ibagué, Colombia

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Ninguna publicación, nacional o extranjera, podrá reproducir ni traducir sus artículos ni sus resúmenes sin previa autorización escrita del editor; sin embargo los usuarios pueden descargar la información contenida en ella, pero deben darle atribución o reconocimiento de propiedad intelectual, deben usarlo tal como está, sin derivación alguna.
Show authors biography
Background: Sleep apnea has been described as a sleep breathing disorder, which in recent years has been gaining importance, being considered a chronic pathology with a high burden of disease. Its study will enable us to fill the gaps in existing knowledge, leading to improved prevention, diagnosis, and treatment that positively impact the quality of life for patients. Objective: To establish the association between sociodemographic and clinical factors in adult patients diagnosed with sleep apnea by polysomnography in a sleep laboratory health prescriber institution (IPS) in the city of Ibagué, Colombia.
Materials and Methods. An analytical cross-sectional study was conducted to explore the relationship between sociodemographic and clinical variables and the outcome of sleep apnea by obtaining the p-value of the Chi-square test of independence and the Odds Ratio (OR), with subsequent adjustment using the Mantel-Haenszel method (MH).
Results. A sample of 128 patients, selected by simple random sampling, was analyzed. Of these, 79.7% (n = 102) presented with sleep apnea, and 54.7% (n = 70) were women. The minimum age of the participants was 18 years. The maximum was 86 years, with an average of 54.5 years; 53.9% (n = 69) had arterial hypertension, and 42.2% (n = 54) were both overweight and obese. Participants older than 55 years presented sleep apnea more frequently than younger ones, with an odds ratio (OR) of 4.86 (95% CI: 1.72-13.73). The remaining variables did not exhibit statistically significant differences. For the sample evaluated, the Berlin questionnaire showed a sensitivity of 74.51% and a specificity of 38.46% for diagnosing sleep apnea compared to polysomnography.
Article visits 411 | PDF visits 154
Downloads
- Darien I. International Classification of Sleep Disorders - Third Edition, text revision (ICSD-3-TR). Am Acad Sleep Med [Internet]. 2023. Disponible en: https://aasm.org/clinical-resources/international-classification-sleep-disorders
- Henry Olivi R. Apnea del sueño: cuadro clínico y estudio diagnóstico. Rev Médica Clínica Las Condes. 2013;24(3):359-73. doi: http://dx.doi.org/10.1016/S0716-8640(13)70173-1 DOI: https://doi.org/10.1016/S0716-8640(13)70173-1
- Broadbent WH. Cheyne-Stokes respiration in cerebral hemorrhage. Lancet. 1877;3:307-9. DOI: https://doi.org/10.1016/S0140-6736(02)21857-7
- Chaudhary BA, Speir WA. Sleep apnea syndromes. South Med J. 1976;75(1):39-45. DOI: https://doi.org/10.1097/00007611-198201000-00011
- Wellman A, Gottlieb Daniel J., Redline S. Harrison Principios de medicina interna. In: Centro Editorial Rosarista. 21 ed. Mc Graw Hill; 2022.
- Hanly C, Laing A, Arnold A. Obstructive Sleep Apnea (OSA): Pathogenesis and Clinical Findings Calgary Guide. The Calgary Guide to understanding disease; 2022 [Internet]. Disponible en: https://calgaryguide.ucalgary.ca/obstructive-sleep-apnea-pathogenesis-and-clinical-findings/
- Mediano O, González Mangado N, Montserrat JM, Alonso-Álvarez ML, Almendros I, Alonso-Fernández A, et al. [Translated article] International consensus document on obstructive sleep apnea. Arch Bronconeumol. 2022;58(1):T52-68. DOI: https://doi.org/10.1016/j.arbres.2021.03.027
- La DES, Cheyne RDE. Los Síndromes de Apnea Central. 2005;17(2):100-3.
- Ginter G, Badr MS. Central sleep apnea. In: Handbook of Clinical Neurology [Internet]. StatPearls Publishing; 2022. p. 93-103. Disponible en: https://www.ncbi.nlm.nih.gov/books/NBK578199/ DOI: https://doi.org/10.1016/B978-0-323-91532-8.00011-2
- Broaddus VC, Schnapp LM, Stapleton RD, Murray JF, Nadel JA, editores. Murray and Nade’s textbook of respiratory medicine. Seventh edition. Philadelphia: Elsevier; 2022. 2 p. ISBN: 9780323655873
- Armengol S, Bernal C, García R. Polisomnografía, poligrafía, oximetría. Requisitos e interpretación de resultados. Man diagnóstico y Ter en Neumol. 2012;(12):195-210.
- Novo-Olivas C, Guitiérrez L, Bribiesca J. Mapeo Electroencefalográfico y Neurofeedback. In 2010. p. 371-412.
- Ogna A, Tobback N, Andries D, Preisig M, Vollenweider P, Waeber G, et al. Prevalence and clinical significance of respiratory effort-related arousals in the general population. J Clin Sleep Med. 2018;14(8):1339-45. DOI: https://doi.org/10.5664/jcsm.7268
- Kumagai H, Sawatari H, Kiyohara Y, Kanoh A, Asada K, Kawaguchi K, et al. Nocturnal hypoxemia is related to morning negative affectivity in untreated patients with severe obstructive sleep apnea. Sci Rep. 2022;12(1):21262. doi: https://doi.org/10.1038/s41598-022-25842-7 DOI: https://doi.org/10.1038/s41598-022-25842-7
- Levi-Valensi P, Weitzenblum E, Rida Z, Aubry P, Braghiroli A, Donner C, et al. Erratum: Sleep-related oxygen desaturation and daytime pulmonary haemodynamics in COPD patients. Eur Respir J. 1992;5(5):301-7. DOI: https://doi.org/10.1183/09031936.93.05030301
- Hidalgo-Martínez P, Lobelo R. Global, latin-american and colombian epidemiology and mortality by obstructive sleep apnea-hypopnea syndrome (OSAHS). Rev Fac Med. 2017;65(1):S17-20.
- Ishikawa O, Oks M. Central Sleep Apnea. Clin Geriatr Med. 2021;37(3):469-81. doi: https://doi.org/10.1016/j.cger.2021.04.009 DOI: https://doi.org/10.1016/j.cger.2021.04.009
- Yurgaky S. JM, Bastidas A, A. J, Montaña JA, Arredondo G. AM. Más allá del molesto ronquido: síndrome de apnea obstructiva del sueño y su peligrosa asociación con el síndrome metabólico. Rev Med. 2011;19(1):37. DOI: https://doi.org/10.18359/rmed.1275
- Nimrod S. Barashi, Rafael E. Ruiz, Lisseth Marín, Paula Ruiz, Sandra Amado, Álvaro J. Ruiz PH. Sindrome de apnea/hipopnea obstructiva del sueño y su asociacion con las enfermedades cardivasculares. Rev Colomb Cardiol. 2015;22(2). DOI: https://doi.org/10.1016/j.rccar.2014.08.009
- Gonzalez L, Castaño J, Herrera V, Jimenez A, Lentijo P, Sierra A, et al. Relación entre HTA y SAHOS y sus factores de riesgo asociados, en población hipertensa de un centro médico. Cali (Colombia) 2008. Investigación Médica; 2014. Disponible en: https://ridum.umanizales.edu.co/handle/20.500.12746/1459
- Salazar-Arenas J, Amado-Garzon S, Ruiz-Gaviria R, Ruiz-Morales A, Ruiz-Severiche L, Hidalgo-Martinez P. Síndrome de apnea/hipopnea obstructiva del sueño y su asociación con las arritmias cardíacas. Una revisión narrativa de la literatura. Rev Colomb Cardiol. 2019;26(2):93-8. DOI: https://doi.org/10.1016/j.rccar.2018.10.014
- Londoño-Palacio N, Machado C. Obstructive sleep apnea-hypopnea syndrome and respiratory diseases. Rev Fac Med. 2017;65(1):S77-80. DOI: https://doi.org/10.15446/revfacmed.v65n1Sup.59526
- Marcelo Miranda C, Rodrigo O. Kuljiš A. Trastornos del sueño en las enfermedades neurodegenerativas. Rev Médica Clínica Las Condes. 2013;24(3):452-62. doi: http://dx.doi.org/10.1016/S0716-8640(13)70181-0 DOI: https://doi.org/10.1016/S0716-8640(13)70181-0
- Johns M. About the ESS – Epworth Sleepiness Scale [Internet]. The Epworth Sleepiness Scale; 1990. Disponible en: https://epworthsleepinessscale.com/about-the-ess/
- Chica-Urzola HL, Escobar-Córdoba F, Eslava-Schmalbach J. Validación de la escala de somnolencia de Epworth. Rev Salud Publica. 2007;9(4):558-67. DOI: https://doi.org/10.1590/S0124-00642007000400008
- Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire To Identify Patients at Risk for the Sleep Apnea Syndrome. Ann Intern Med. 1999;131(7):485-91. DOI: https://doi.org/10.7326/0003-4819-131-7-199910050-00002
- Polanía-Dussan IG, Escobar-Córdoba F, Eslava-Schmalbach J, Netzer NC. Colombian validation of the Berlin questionnaire / Validación colombiana del cuestionario de Berlín. Rev Fac Med. 2013;61(3):231-8.
- Saldías P. F, Leiva R. I, Salinas R. G, Stuardo T. L. Estudios de prevalencia del síndrome de apneas obstructivas del sueño en la población adulta. Rev Chil enfermedades Respir. 2021;37(4):303-16. DOI: https://doi.org/10.4067/s0717-73482021000300303
- Schwarz EI, Schiza S. Sex differences in sleep and sleep-disordered breathing. Curr Opin Pulm Med. 2024;30(6):593-9. DOI: https://doi.org/10.1097/MCP.0000000000001116
- Departamento Administrativo Nacional de Estadistica DANE. Encuesta Nacional de Consumo de Sustancias [Internet]. Vol. 3, Ministerio de Justicia, Gobierno de Colombia; 2019. p. 1-34. Disponible en: https://www.dane.gov.co/files/investigaciones/boletines/encspa/bt-encspa-2019.pdf
- González S, Sarmiento OL, Lozano Ó, Ramírez A, Grijalba C. Niveles de actividad física de la población colombiana: Desigualdades por sexo y condición socioeconómica. Biomédica. 2014;34(3):447-59. DOI: https://doi.org/10.7705/biomedica.v34i3.2258
- Hou H, Zhao Y, Yu W, Dong H, Xue X, Ding J, et al. Association of obstructive sleep apnea with hypertension: A systematic review and meta-analysis. J Glob Health. 2018;8(1). doi: https://doi.org/10.7189/jogh.08.010405 DOI: https://doi.org/10.7189/jogh.08.010405
- Dacal Quintas R, Tumbeiro Novoa M, Alves Pérez MT, Santalla Martínez ML, Acuña Fernández A, Marcos Velázquez P. Síndrome de apnea-hipopnea del sueño en pacientes normopeso: características y comparación con pacientes con sobrepeso y obesidad. Arch Bronconeumol. 2013;49(12):513-7. DOI: https://doi.org/10.1016/j.arbres.2013.05.005
- Peñafiel FS, Poniachik JG, López AC, Monasterio JU, Patiño OD. Accuracy of sleep questionnaires for obstructive sleep apnea syndrome screening. Rev Med Chil. 2018;146(10):1123-34. doi: http://dx.doi.org/10.4067/S0034-98872018001001123 DOI: https://doi.org/10.4067/S0034-98872018001001123
- Cancino Q. V, Rivera T. E, Cancino Q. V, Rivera T. E. Symptoms during sleep among patients with obstructive sleep apnea. Rev Med Chil. 2018;146(4):470-8. doi: http://dx.doi.org/10.4067/s0034-98872018000400470 DOI: https://doi.org/10.4067/s0034-98872018000400470