Bronchiectasis due to pulmonary tuberculosis in a Hospital in the Peruvian Jungle
Bronquiectasias por tuberculosis pulmonar en un hospital de la selva peruana

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Ninguna publicación, nacional o extranjera, podrá reproducir ni traducir sus artículos ni sus resúmenes sin previa autorización escrita del editor; sin embargo los usuarios pueden descargar la información contenida en ella, pero deben darle atribución o reconocimiento de propiedad intelectual, deben usarlo tal como está, sin derivación alguna.
Show authors biography
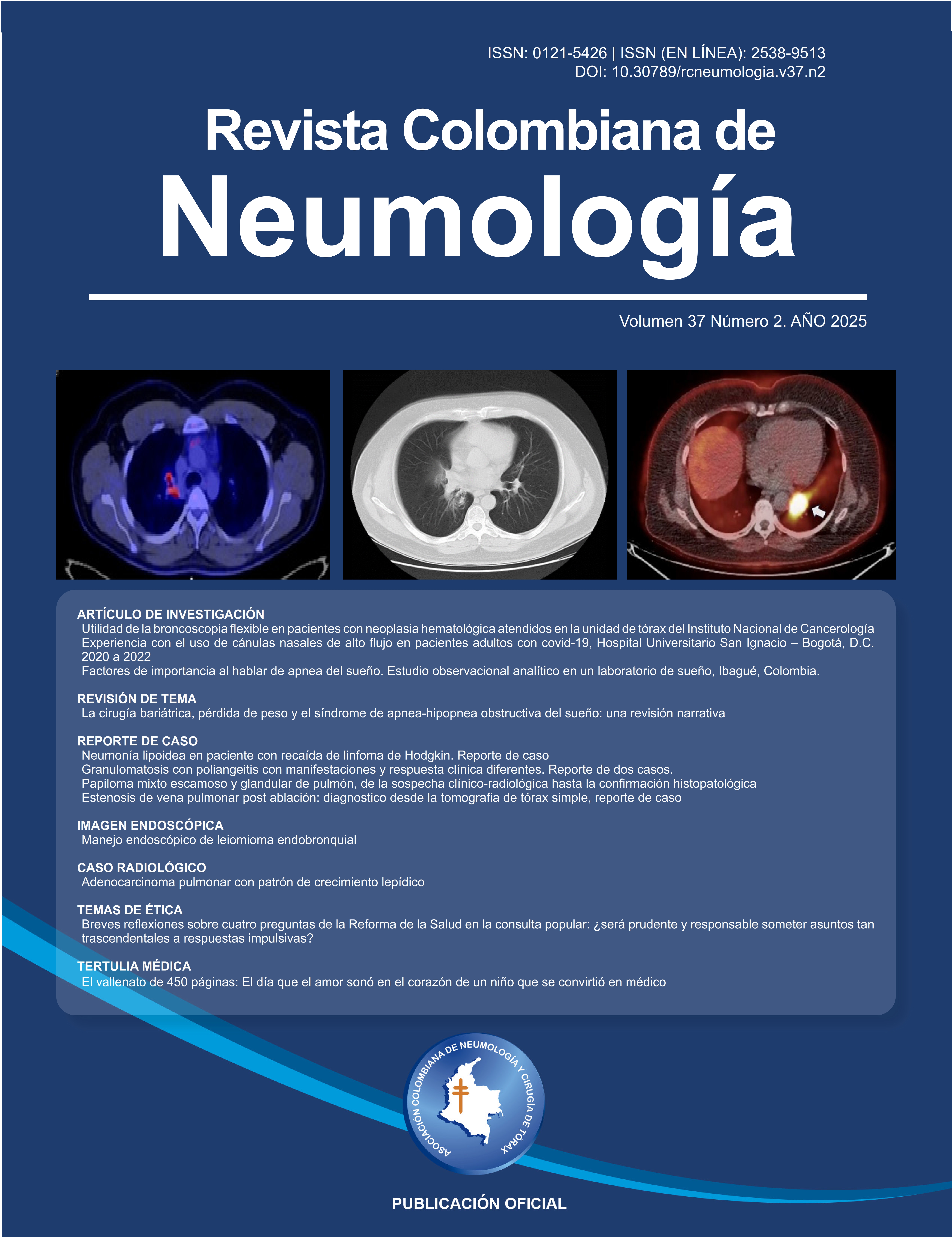
Introduction: Pulmonary tuberculosis is a disease with a high prevalence and incidence in Peru. In 2018, the San Martín region had an annual incidence of 34 per 100,000 inhabitants. It is estimated that half of these patients will develop a complication of pulmonary tuberculosis throughout their lives, with bronchiectasis being among the most common.
Objective: To characterize sequelae of bronchiectasis due to treated and cured pulmonary tuberculosis in patients treated at Hospital II-2 Tarapoto from January 2017 to December 2020.
Materials and methods: This study employed observational, descriptive, cross-sectional, and retrospective research, utilizing medical records to characterize post-pulmonary tuberculosis bronchiectasis as a foundation for future research on a little-studied disease. Forty-one cases of bronchiectasis were studied in patients treated for and cured of pulmonary tuberculosis at Hospital II-2 Tarapoto from January 2017 to December 2020.
Results: The most common age group was adults between 30 and 64 years (68.3%), more often in women (58.5%), presenting a normal weight according to BMI (68.3%), and were diagnosed with bronchiectasis more regularly between 1 and 11 years after discharge with cured pulmonary tuberculosis (63.4%). The main symptoms were productive cough (82.9%), dyspnea (43.9%), and chest pain (41.5%). The characteristic sign was subcrackly breath sounds (24.4 %). Both imaging studies were used at nearly equal frequencies when establishing the diagnosis (chest CT in 51.2% and chest X-ray in 48.8%). Bronchiectasis was most frequently affected in the right lung (36.6%) and upper lobes (39%). The most common type of bronchiectasis, as determined by computed tomography (CT), was cylindrical (57.1%). The most frequently isolated bacterial pathogens were Enterobacter gergoviae (24.3%) and Klebsiella pneumoniae (13.5%).
Conclusions: Protocols should be developed to achieve a timelier diagnosis, including guidelines for routine follow-up in patients who have completed tuberculosis treatment and have been discharged to provide early treatment.
Article visits 233 | PDF visits 19
Downloads
- Jaramillo Peralta IB. Evaluación funcional respiratoria en pacientes con tuberculosis pulmonar secuelar del Hospital Nacional Arzobispo Loayza del 2013 [Internet] [Trabajo de investigación]. Universidad Nacional Mayor de San Marcos [Lima - Perú]; 2014 [citado 13 de junio de 2023]. Disponible en: https://hdl.handle.net/20.500.12672/13272
- Benites López KE. Factores asociados a tuberculosis multidrogorresistente de los Establecimientos de Salud de Piura 2015 - 2018 [Internet] [Tesis]. Universidad Privada Antenor Orrego [Piura - Perú]; 2020 [citado 13 de junio de 2023]. Disponible en: https://hdl.handle.net/20.500.12759/6070
- Ministerio de Salud. Sala situacional de Tuberculosis en el Perú [Internet]. Perú; 2019 [citado 13 de junio de 2023]. Disponible en: https://www.dge.gob.pe/portal/docs/tools/teleconferencia/2019/SE122019/04.pdf
- Benito Condor B, Contreras Camarena C, Justo Calle R, Llanos Tejada F, Salas López J, Jave Castillo H. Factores asociados a hemoptisis en pacientes con tuberculosis pulmonar en el Hospital Nacional Dos de Mayo, Lima - Perú. An Fac med [Internet]. 2020 [citado 13 de junio de 2023];81(4):398-403. Disponible en: https://doi.org/10.15381/anales.v81i4.18748
- Llanos-Tejada F, Tamayo-Alarcón R. Bronquiectasias secundarias a Tuberculosis pulmonar en pacientes de un hospital general. Rev Med Hered [Internet]. 2018 [citado 13 de junio de 2023];29:232-7. Disponible en: http://dx.doi.org/https://doi.org/10.20453/rmh.v29i4.3448
- Romero Marín MP, Romero Rondon SK, Sánchez Robayo J, Santamaria-Alza Y, Mendoza Herrera T, Bolivar Grimaldos F. Secuelas estructurales y funcionales de tuberculosis pulmonar: una revisión de tema. Revista Americana de Medicina Respiratoria [Internet]. 2016 [citado 13 de junio de 2023];16(2):163-9. Disponible en: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S1852-236X2016000200007&lng=es.
- Hsu D, Irfan M, Jabeen K, Iqbal N, Hasan R, Migliori GB, et al. Post tuberculosis treatment infectious complications. International Journal of Infectious Diseases. 1 de marzo de 2020;92:S41-5.
- Uribe A, Molina G, Resurrección V, Figueroa M. Bronquiectasias y Limitación Funcional en la Tuberculosis Pulmonar Curada. Anales de la Facultad de Medicina [Internet]. 2000;61:309-14. Disponible en: http://www.redalyc.org/articulo.oa?id=37961409
- Sahin H, Naz I, Susam S, Erbaycu A, Olcay S. The effect of the presence and severity of bronchiectasis on the respiratory functions, exercise capacity, dyspnea perception, and quality of life in patients with chronic obstructive pulmonary disease. Ann Thorac Med [Internet]. 2020;15(1):26-32.
- Jordan TS, Spencer EM, Davies P. Tuberculosis, bronchiectasis and chronic airflow obstruction. Respirology. 2010;15(4):623-8. doi: https://doi.org/10.1111/j.1440-1843.2010.01749.x
- Gissel TN, Hvass M, Fly J, Børsting K, Birring SS, Spinou A, et al. Translation and linguistic validation of the Bronchiectasis Health Questionnaire (BHQ) into Danish. Dan Med J [Internet]. 2020 [citado 13 de junio de 2023];67(3):1-4. Disponible en: http://ugeskriftet.dk/dmj/translation-and-linguistic-validation-bronchiectasis-health-questionnaire-bhq-danish
- Da Silva Moreira J, Da Silva Porto N, Peixoto Camargo J de J, Felicetti JC, Guerreiro Cardoso PF, Schneider Moreira AL, et al. Bronchiectasis: diagnostic and therapeutic features A study of 170 patients. J Pneumol [Internet]. 2003 [citado 13 de junio de 2023];29(5):258-63. Disponible en: https://www.scielo.br/j/jpneu/a/Qhk4XtwsmQxQFy5Dmnw9Cwt/?format=pdf
- Poma Torres D. Estudio prospectivo de bronquiectasias, etiología y diagnóstico diferencial en pacientes admitidos en el Hospital Isidro Ayora en el servicio de clínica: Durante el periodo mayo - octubre 2011 [Internet] [Tesis]. Universidad Nacional de Loja [Loja - Ecuador]; 2012 [citado 13 de junio de 2023]. Disponible en: http://dspace.unl.edu.ec/jspui/handle/123456789/6564
- Ocampo ML, Salmón JAA, Noguera VD, Zabala OC. Bronquiectasias: Revisión bibliográfica. Revista de Posgrado de la VIa Cátedra de Medicina [Internet]. 2008 [citado 13 de junio de 2023];182:16-9. Disponible en: https://studylib.es/doc/5969028/bronquiectasias--revision-bibliografica
- Habesoglu MA, Ugurlu AO, Eyuboglu FO. Clinical, radiologic, and functional evaluation of 304 patients with bronchiectasis. Annals of Thoracic Medicine. 2011;6:131-6. doi: https://doi.org/10.4103/1817-1737.82443
- Martínez-García MÁ, Máiz L, Olveira C, Girón RM, de la Rosa D, Blanco M, et al. Normativa sobre la valoración y el diagnóstico de las bronquiectasias en el adulto. Arch Bronconeumol. 1 feb 2018;54(2):79-87. doi: https://doi.org/10.1016/j.arbres.2017.07.015
- Romero S, Graziani D. Bronquiectasias. Medicine - Programa de Formación Médica Continuada Acreditado. 2018 [citado el 19 de junio de 2025];12(63):3691–8. doi: https://doi.org/10.1016/j.med.2018.09.010
- Naidich DP, McCauley DI, Khouri NF, Stitik FP, Siegelman SS. Computed Tomography of Bronchiectasis. J Comput Assist Tomogr. 1982;6(3):437-44. doi: https://doi.org/10.1097/00004728-198206000-00001
- Dhar R, Singh S, Talwar D, Mohan M, Tripathi SK, Swarnakar R, et al. Bronchiectasis in India: results from the European Multicentre Bronchiectasis Audit and Research Collaboration (EMBARC) and Respiratory Research Network of India Registry. Lancet Glob Health [Internet]. 1 de septiembre 2019 [citado 13 de junio de 2023] ;7(9):e1269-79. Disponible en: https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(19)30327-4/fulltext
- Llanos-Tejada F. Alteraciones espirométricas en pacientes con secuela de tuberculosis pulmonar. Rev Med Hered [Internet]. 2010 [citado 13 de junio de 2023];21:77-83. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1018-130X2010000200005
- Bak SH, Kim S, Hong Y, Heo J, Lim MN, Kim WJ. Quantitative computed tomography features and clinical manifestations associated with the extent of bronchiectasis in patients with moderate-to-severe COPD. Int J Chron Obstruct Pulmon Dis. mayo de 2018;13:1421-31. doi: https://doi.org/10.2147/copd.s157953
- Jin J, Li S, Yu W, Liu X, Sun Y. Emphysema and bronchiectasis in COPD patients with previous pulmonary tuberculosis: Computed tomography features and clinical implications. International Journal of COPD. 24 de enero de 2018;1:375-84. Doi: https://doi.org/10.2147/copd.s152447
- Nega B, Ademe Y, Tizazu A. Bronchiectasis: Experience of Surgical Management at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Ethiop J Health Sci. 1 de julio de 2019;29(4):471-6. doi: https://doi.org/10.4314/ejhs.v29i4.8
- Mantilla-Florez YF, Tuta-Quintero E, Brito-Rodríguez AJ, Clavijo-Moreno LC. Candidiasis y Candida albicans. Bol Malariol Salud Ambient. 1 de julio de 2021;61(3):391-400. doi: https://doi.org/10.52808/bmsa.7e5.613.003
- Máiz L, Nieto R, Cantón R, Gómez G de la Pedrosa E, Martinez-García MÁ. Fungi in Bronchiectasis: A Concise Review. Int J Mol Sci. el 4 de enero de 2018;19(1):142. doi: https://doi.org/10.3390/ijms19010142
- Costa JC, Machado JN, Ferreira C, Gama J, Rodrigues C. The Bronchiectasis Severity Index and FACED score for assessment of the severity of bronchiectasis. Pulmonology. 2018;24(3):149–54. doi: https://doi.org/10.1016/j.rppnen.2017.08.009
- Girón RM, Martínez-Vergara A, Oscullo Yépez G, Martinez-García MA. Las bronquiectasias como enfermedad compleja. Open Respiratory Archives. el 1 de julio de 2020;2(3):226–34. doi: https://doi.org/10.1016/j.opresp.2020.05.007
- Perú. Ministerio de Salud. Resolución Ministerial 546-2011. NTS Nº 021-MINSA / DGSP-V.03 Norma Técnica de Salud. “Categorías de establecimientos del sector salud” [Internet]. 2011. Disponible en: https://cdn.gacetajuridica.com.pe/laley/NORMA%20T%C3%89CNICA%20DE%20SALUD%20N%C2%BA021-MINSA-DGSP-V.03_LALEY.pdf