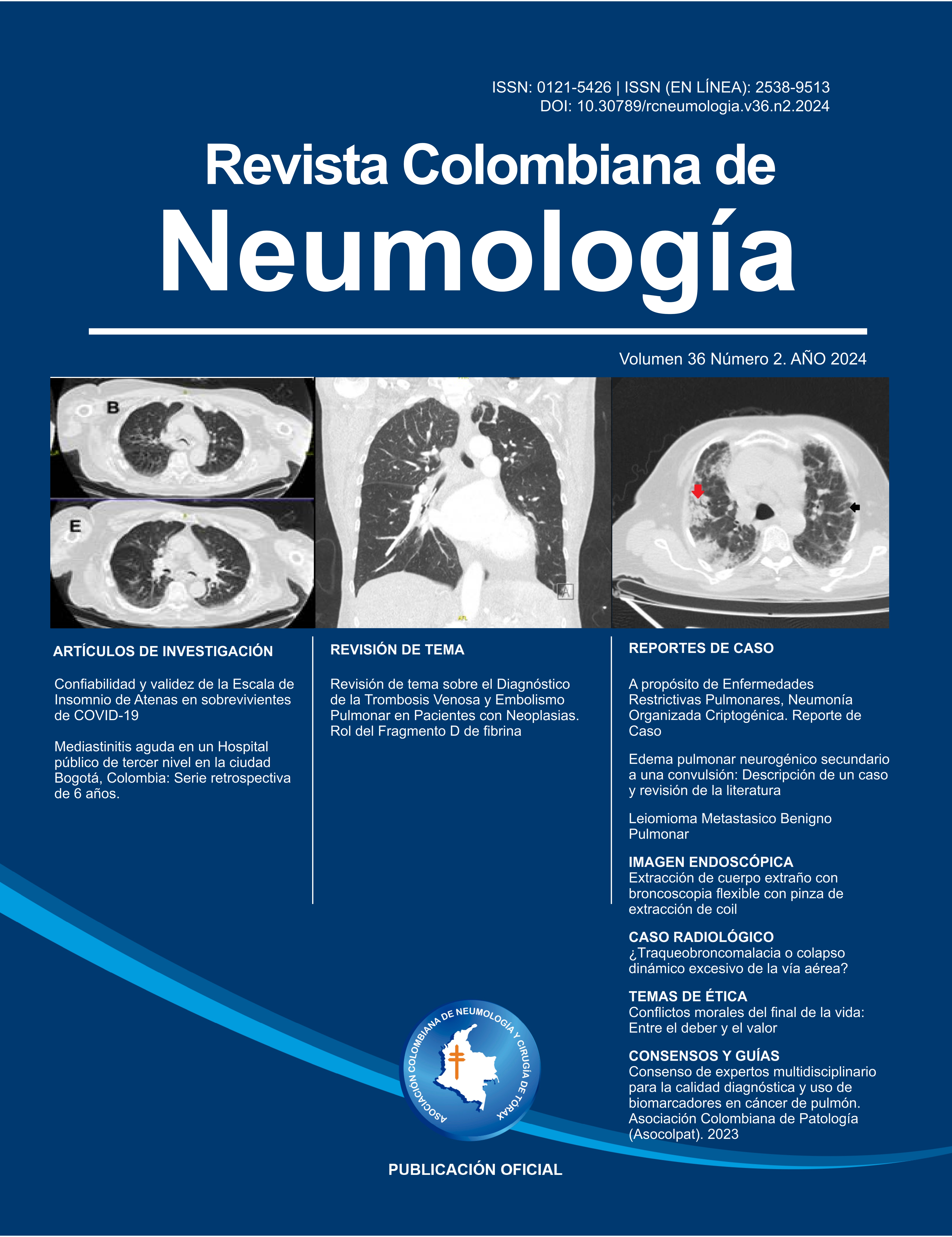
Revisión de los métodos diagnósticos de la Trombosis Venosa Profunda y Embolismo Pulmonar. Rol del Fragmento D de fibrina
Review of topic on the Diagnosis of Venous Thrombosis and Pulmonary Embolism in Patients with Neoplasms. Role of fibrin Fragment D

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
Ninguna publicación, nacional o extranjera, podrá reproducir ni traducir sus artículos ni sus resúmenes sin previa autorización escrita del editor; sin embargo los usuarios pueden descargar la información contenida en ella, pero deben darle atribución o reconocimiento de propiedad intelectual, deben usarlo tal como está, sin derivación alguna.
Mostrar biografía de los autores
Introducción. La enfermedad tromboembólica venosa, representada por la trombosis venosa profunda y el embolismo pulmonar, constituye una patología de alta prevalencia tanto en pacientes intra como extra hospitalarios, con un número cada vez más amplio de factores de riesgo asociados, algunos de ellos no representados en las escalas de riesgo y pronóstico implementadas en la actualidad. Es el caso de las patologías neoplásicas de órgano sólido y hematológicas, las cuales se han asociado con falsos positivos en el resultado de pruebas como el dímero D y eventos trombóticos recurrentes, lo cual dificulta establecer un algoritmo de diagnóstico y un tiempo de anticoagulación, luego de la resolución del evento trombótico inicial.
Objetivo. Documentar el uso de ecografía doppler de compresión de miembros inferiores, la angioresonancia pulmonar (ARP) y la angiotomografía de tórax con mapa de yodo (ATMY) en pacientes con cáncer y sospecha de eventos trombóticos, tienen un valor predictivo negativo comparable al dímero D en ausencia del cáncer, por ende, se requiere mayor implementación de dichas estrategias diagnósticas en los algoritmos de estos pacientes.
Materiales y métodos. Se realizó una búsqueda de la literatura publicada en las bases de datos Medline (PubMed), OncoWeb y CancerLit (HealthGate), con los siguientes términos MeSH en inglés: pulmonary embolism (embolismo pulmonar), venous thrombosis (trombosis venosa), neoplasms (neoplasia), diagnosis (diagnóstico), D-dimer or fibrin fragment D (dímero D o fragmento D de fibrina), y epidemiology (epidemiología).
Visitas del artículo 541 | Visitas PDF 364
Descargas
- Patel P, Patel P, Bhatt M, Braun C, Begum H, Nieuwlaat R, et al. Systematic review and meta-analysis of outcomes in patients with suspected deep vein thrombosis. Blood Advances. 2020; 4(12): 2779 – 2788. doi:10.1182/bloodadvances.2020001558 DOI: https://doi.org/10.1182/bloodadvances.2020001558
- Germini F, Zarabi S, Eventov M, Turcotte M, Li M, de Wit K. Pulmonary embolism prevalence among emergency department cohorts: A systematic review and meta-analysis by country of study J Thromb Haemost. 2021; 19: 173–185. doi: 10.1111/jth.15124 DOI: https://doi.org/10.1111/jth.15124
- Klemen N, Feingold P, Hashimoto B, Wang M, Kleyman S, Brackett A, et al. Mortality risk associated with venous thromboembolism: a systematic review and Bayesian meta-analysis. The Lancet Haematology. 2020; 7: 583-593. doi: 10.1016/S2352-3026(20)30211-8 DOI: https://doi.org/10.1016/S2352-3026(20)30211-8
- Gao Y, Wang Y, Cao X, Wang X, Zheng Q, Zhao H, et al. Rapid prediction of deterioration risk among non-high-risk patients with acute pulmonary embolism at admission: An imaging tool. International Journal of Cardiology 338. 2021 229–236. doi: 10.1016/j.ijcard.2021.06.013 DOI: https://doi.org/10.1016/j.ijcard.2021.06.013
- Rahmani J, Roudsari A, Bawadi H, et al, Relationship between body mass index, risk of venous thromboembolism and pulmonary embolism: A systematic review and dose-response meta-analysis of cohort studies among four million participants. Thrombosis Research. 2020. doi: 10.1016/j.thromres.2020.05.014 DOI: https://doi.org/10.1016/j.thromres.2020.05.014
- Jara-Palomares L, van Es N, Praena-Fernandez J, Le Gal G, Otten H, Robin P, et al. Relationship between type of unprovoked venous thromboembolism and cancer location: An individual patient data meta-analysis. Thrombosis Research. 2019; 176: 79–84. doi: 10.1016/j.thromres.2019.02.011 DOI: https://doi.org/10.1016/j.thromres.2019.02.011
- Meyer H, Wienke A, Surov A. Incidental pulmonary embolism in oncologic patients—a systematic review and meta-analysis. Support Care Cancer. 2021; 29: 1293–1302. doi: 10.1007/s00520-020-05601-y DOI: https://doi.org/10.1007/s00520-020-05601-y
- Giustozzi M, Connors J, Ruperez A, Szmit S, Falvo N, Cohen A, et al. Clinical characteristics and outcomes of incidental venous thromboembolism in cancer patients: Insights from the Caravaggio study. J Thromb Haemost. 2021;19:2751–2759. doi: 10.1111/jth.15461 DOI: https://doi.org/10.1111/jth.15461
- Mulder F, Di Nisio M, 3, Ay C, Carrier M, Bosch F, Segers S, et al. Clinical implications of incidental venous thromboembolism in cancer patients. Eur Respir J 2020; 55: 1901697. doi: 10.1183/13993003.01697-2019 DOI: https://doi.org/10.1183/13993003.01697-2019
- Nisio D, Candeloro M, Rutjes A, Porreca E. Venous thromboembolism in cancer patients receiving neoadjuvant chemotherapy: a systematic review and meta-analysis. Journal of Thrombosis and Haemostasis. 2018; 16: 1336–1346. doi: 10.1111/jth.14149 DOI: https://doi.org/10.1111/jth.14149
- Robertson L, Yeoh SE, Broderick C, Stansby G, Agarwal R. Effect of testing for cancer on cancer- or venous thromboembolism (VTE)-related mortality and morbidity in people with unprovoked VTE. Cochrane Database of Systematic Reviews. 2018; 11 (CD010837). doi: 10.1002/14651858.CD010837.pub4 DOI: https://doi.org/10.1002/14651858.CD010837.pub4
- Bao Y, Gao B, Yan P, Tian L, Yang K. The effectiveness and safety of thromboprophylaxis in cancer patients based on Khorana score: a meta analysis and systematic review of randomized controlled trials. Clinical and Translational Oncology. 2020; 22(11):1992-2001. doi: 10.1007/s12094-020-02336-4 DOI: https://doi.org/10.1007/s12094-020-02336-4
- Galanaud J-P, Blaise S, Sevestre MA, Terrisse H, Pernod G, Gaillard C, et al. Long-term outcomes of isolated superficial vein thrombosis in patients with active cancer. Thrombosis Research. 2018; 171:179-186. doi: 10.1016/j.thromres.2018.04.013 DOI: https://doi.org/10.1016/j.thromres.2018.04.013
- Chopard R, Ehlers I, Piazza G. Diagnosis and Treatment of Lower Extremity Venous Thromboembolism - A Review. JAMA. 2020;324(17):1765-1776. doi: 10.1001/jama.2020.17272 DOI: https://doi.org/10.1001/jama.2020.17272
- Ntinopoulou P, Ntinopoulou E, Papathanasiou I.V, Fradelos E.C, Kotsiou O, Roussas N, et al. Obesity as a Risk Factor for Venous Thromboembolism Recurrence: A Systematic Review. Medicina. 2022, 58: 1290-1304 doi: 10.3390/medicina58091290 DOI: https://doi.org/10.3390/medicina58091290
- Hayssen H, Cires-Drouet R, Englum B, Nguyen P, Sahoo S, Mayorga-Carlin M, et al. Systematic review of venous thromboembolism risk categories derived from Caprini score. J Vasc Surg Venous Lymphat Disord 2022;10:1401-1409. doi: 10.1016/j.jvsv.2022.05.003 DOI: https://doi.org/10.1016/j.jvsv.2022.05.003
- Bhatt M, Braun C, Patel P, Patel P, Begum H, Wiercioch W, et al. Diagnosis of deep vein thrombosis of the lower extremity: a systematic review and meta-analysis of test accuracy. Blood advances. 2020; 4(7): 1250-1264. doi: 10.1182/bloodadvances.2019000960 DOI: https://doi.org/10.1182/bloodadvances.2019000960
- Patel P, Braun C, Patel P, Bhatt M, Begum H, Wiercioch W, et al. Diagnosis of deep vein thrombosis of the upper extremity: a systematic review and meta-analysis of test accuracy. Blood advances. 2020; 4(11): 2516-2522. doi: 10.1182/bloodadvances.2019001409 DOI: https://doi.org/10.1182/bloodadvances.2019001409
- Takada T, Van Doorn S, Parpia S, de Wit K, Anderson D, Stevens S. Diagnosing deep vein thrombosis in cancer patients with suspected symptoms: An individual participant data meta-analysis. J Thromb Haemost. 2020; 18: 2245–2252. doi: 10.1111/jth.14900 DOI: https://doi.org/10.1111/jth.14900
- Robertson L, Broderick C, Yeoh SE, Stansby G. Effect of testing for cancer on cancer- or venous thromboembolism (VTE)-related mortality and morbidity in people with unprovoked VTE. Cochrane Database of Systematic Reviews. 2021, 10 (CD010837). doi: 10.1002/14651858.CD010837.pub4 DOI: https://doi.org/10.1002/14651858.CD010837.pub5
- Ordieres-Ortega L, Demelo-Rodríguez P, Galeano-Valle F, et al. Predictive value of D-dimer testing for the diagnosis of venous thrombosis in unusual locations: A systematic review. Thromb Res. 202; 189: 5-12. doi: 10.1016/j.thromres.2020.02.009 DOI: https://doi.org/10.1016/j.thromres.2020.02.009
- Aguilara C, Sarborib M, D’Angeloc A, Kabrheld C, Grocee J, de Maistref E, et al. Validation of the STA-Liatest DDi assay for exclusion of proximal deep vein thrombosis according to the latest Clinical and Laboratory Standards Institute/Food and Drug Administration guideline: results of a multicenter management study. Blood Coagul Fibrinolysis. 2018; 29: 562–566. doi: 10.1097/MBC.0000000000000750 DOI: https://doi.org/10.1097/MBC.0000000000000750
- Kraaijpoel N, Carrier M, Le Gal G, McInnes MDF, Salameh J-P, McGrath TA, et al. Diagnostic accuracy of three ultrasonography strategies for deep vein thrombosis of the lower extremity: A systematic review and meta-analysis. PLoS ONE. 2020; 15(2): e0228788. doi: 10.1371/journal.pone.0228788 DOI: https://doi.org/10.1371/journal.pone.0228788
- Lee JH, Lee SH, Yun SJ. Comparison of 2-point and 3-point point-of-care ultrasound techniques for deep vein thrombosis at the emergency department. A meta-analysis. Medicine. 2019; 98(22): 1-11. doi: 10.1097/MD.0000000000015791 DOI: https://doi.org/10.1097/MD.0000000000015791
- Tini G, Moriconi A, Ministrini S, Zullo V, Venanzi E, Mondovecchio G, et al. Ultrasound screening for asymptomatic deep vein thrombosis in critically ill patients: a pilot trial. Internal and Emergency Medicine. 2022; 17: 2269–2277. doi: 10.1007/s11739-022-03085-8 DOI: https://doi.org/10.1007/s11739-022-03085-8
- Zhang Y, Xia H, Wang Y, Chen L, Li S, Hussein IA, et al. The rate of missed diagnosis of lower-limb DVT by ultrasound amounts to 50% or so in patients without symptoms of DVT. Medicine. 2019; 98 (37): e17103. doi: 10.1097/MD.0000000000017103 DOI: https://doi.org/10.1097/MD.0000000000017103
- Van Dam L,1, Dronkers C, Gautam G, Eckerbom A, Ghanima W, Gleditsch J, et al. Magnetic resonance imaging for diagnosis of recurrent ipsilateral deep vein thrombosis. Blood. 2020; 135(16):1377-1385. doi: 10.1182/blood.2019004114 DOI: https://doi.org/10.1182/blood.2019004114
- Zhang Y, Begum H, Grewal H, Etxeandia-Ikobaltzeta I, Morgano G, Khatib R, et al. Cost-effectiveness of diagnostic strategies for venous thromboembolism: a systematic review. Blood advances. 2022; 6 (2): 544-567. doi: 10.1182/bloodadvances.2020003576 DOI: https://doi.org/10.1182/bloodadvances.2020003576
- Barco S, Ende-Verhaar Y, Becattini C, Jimenez D, Lankeit M, Huisman M, et al. Differential impact of syncope on the prognosis of patients with acute pulmonary embolism: a systematic review and meta-analysis. European Heart Journal. 2018; 39: 4186–4195. doi: 10.1093/eurheartj/ehy631 DOI: https://doi.org/10.1093/eurheartj/ehy631
- Maanen R, Trinks-Roerdink E, Rutten F, Geersing G. A systematic review and meta-analysis of diagnostic delay in pulmonary embolism. European Journal Of General Practice. 2022; 28(1): 165–172. doi: 10.1080/13814788.2022.2086232 DOI: https://doi.org/10.1080/13814788.2022.2086232
- Zuin M, Rigatelli G, Zuliani G, Adami A, Zonzin P, Roncon L. Seizures as the first clinical manifestation of acute pulmonary embolism: an underestimate issue in neurocritical care. Neurol Sci. 2020; 41(6): 1427-1436. doi: 10.1007/s10072-020-04275-y DOI: https://doi.org/10.1007/s10072-020-04275-y
- Jiménez D, Agustí A, Tabernero E, Jara-Palomares L, Hernando A, Ruiz-Artacho P, et al. Effect of a Pulmonary Embolism Diagnostic Strategy on Clinical Outcomes in Patients Hospitalized for COPD Exacerbation. A Randomized Clinical Trial. JAMA. 2021; 326 (13): 1277-1285. doi: 10.1001/jama.2021.14846 DOI: https://doi.org/10.1001/jama.2021.14846
- Lahera A, Richardsb G. Cardiac arrest due to pulmonary embolism. Indian Heart Journal 70. 2018: 731–735. doi: 10.1016/j.ihj.2018.01.014 DOI: https://doi.org/10.1016/j.ihj.2018.01.014
- Stalls M, Takada T, Kraaijpoel N, Es N, Büller H, Courtney M, et al. Safety and Efficiency of Diagnostic Strategies for Ruling Out Pulmonary Embolism in Clinically Relevant Patient Subgroups. A Systematic Review and Individual-Patient Data Meta-analysis. Ann Intern Med. 2022; 175: 244-255. doi: 10.7326/M21-2625 DOI: https://doi.org/10.7326/M21-2625
- Geersing G, Takada T, Klok F, Bu ̈lle R, Courtney M, Freund Y, et al. Ruling out pulmonary embolism across different healthcare settings: A systematic review and individual patient data meta-analysis. 2022. PLoS Med; 19 (1): e1003905. doi: 10.1371/journal.pmed.1003905 DOI: https://doi.org/10.1371/journal.pmed.1003905
- Patel P, Patel P, Bhatt M, Braun C, Begum H, Wiercioch W, et al. Systematic review and meta-analysis of test accuracy for the diagnosis of suspected pulmonary embolism. Blood advances. 2020; 4 (18): 4296-4311. doi: 10.1182/bloodadvances.2019001052 DOI: https://doi.org/10.1182/bloodadvances.2019001052
- Wang Y, Feng Y, Du R, Yang X, Huang J, Mao H. Prognostic Performance of Hestia Criteria in Acute Pulmonary Embolism: A Systematic Review and Meta-Analysis. Clinical and Applied Thrombosis/Hemostasis. 2022; 28: 1-11. doi: 10.1177/10760296221126173 DOI: https://doi.org/10.1177/10760296221126173
- El-Menyara A, Sathiana B, Al-Thanic H. Elevated serum cardiac troponin and mortality in acute pulmonary embolism: Systematic review and meta-analysis. Respiratory Medicine. 2019; 157: 26–35. doi: 10.1016/j.rmed.2019.08.011 DOI: https://doi.org/10.1016/j.rmed.2019.08.011
- Zuin M, Rigatelli G, Turchetta S, Zonzin P, Zuliani G, Roncon L. Left atrial size measured on CT pulmonary angiography: another parameter of pulmonary embolism severity? A systematic review. Journal of Thrombosis and Thrombolysis. 2020; 50 (1): 181-189. doi: 10.1007/s11239-019-01994-8 DOI: https://doi.org/10.1007/s11239-019-01994-8
- Chornenki N, Poorzargar K, Shanjer M, Mbuagbaw L, Delluc A, Crowther M, et al. Detection of right ventricular dysfunction in acute pulmonary embolism by computed tomography or echocardiography: A systematic review and meta-analysis. J Thromb Haemost. 2021; 19: 2504–2513. doi: 10.1111/jth.15453 DOI: https://doi.org/10.1111/jth.15453
- Kagima J, Stolbrink M, Masheti S, Mbaiyani C, Munubi A, Joekes E, et al. Diagnostic accuracy of combined thoracic and cardiac sonography for the diagnosis of pulmonary embolism: A systematic review and meta-analysis. PLoS ONE 15(9): e0235940. doi: 10.1371/journal.pone.0235940 DOI: https://doi.org/10.1371/journal.pone.0235940
- Chen W, Xu K, Li Y, Hao M, Yang Y, Liu X, et al. Clinical value of thoracic ultrasonography in the diagnosis of pulmonary embolism: a systematic review and meta-analysis. Med Ultrason. 2022; 24 (2): 226-234. doi: 10.11152/mu-3049 DOI: https://doi.org/10.11152/mu-3049
- Ransome W, Dizonb J, Guerreroa K, Chauc M. Diagnostic test accuracy of imaging modalities for adults with acute pulmonary embolism: A systematic review and meta-analysis. Journal of Medical Imaging and Radiation Sciences. 2023; 54 (1): 178–194. doi: 10.1016/j.jmir.2022.11.003 DOI: https://doi.org/10.1016/j.jmir.2022.11.003
- Andruchow J, Grigat D, McRae A, Innes G, Vatanpour S, Wang D, et al. Decision support for computed tomography in the emergency department: a multicenter cluster‐randomized controlled trial. Canadian Journal of Emergency Medicine. 2021; 23: 631–640. doi: 10.1007/s43678-021-00170-3 DOI: https://doi.org/10.1007/s43678-021-00170-3
- Dissaux B, Le Floch P, Robin P, Bourhis D, Couturaud F, Salaun P, et al. Pulmonary perfusion by iodine subtraction maps CT angiography in acute pulmonary embolism: comparison with pulmonary perfusion SPECT (PASEP trial). Eur Radiol. 2020; 30(9): 4857-4864. doi: 10.1007/s00330-020-06836-3 DOI: https://doi.org/10.1007/s00330-020-06836-3
- Sosa D, Lehr A, Zhao H, Roth S, Lakhther V, Bashir R, et al. Impact of pulmonary embolism response teams on acute pulmonary embolism: a systematic review and meta-analysis. Eur Respir Rev 2022; 31: 220023. doi: 10.1183/16000617.0023-2022 DOI: https://doi.org/10.1183/16000617.0023-2022
- Hua X, Han S-H, Wei S-Z, Wu Y, Sha J, ZhuX-L. Clinical features of pulmonary embolism in patients with lung cancer: A meta-analysis. PLoS ONE. 2019; 14(9): e0223230. doi: 10.1371/journal.pone.0223230 DOI: https://doi.org/10.1371/journal.pone.0223230
- Lu Y, Zhang L, Zhang O, Zhang Y, Chen D, Lou J, Jiang J, Ren C. The association of D-dimer with clinicopathological features of breast cancer and its usefulness in differential diagnosis: A systematic review and meta-analysis. PLoS ONE. 2019; 14(9): e0221374. doi: 10.1371/journal.pone.0221374 DOI: https://doi.org/10.1371/journal.pone.0221374
- Lin Y, Liu Z, Qiu Y, Zhang J, Wu H, Liang R. Clinical significance of plasma D-dimer and fibrinogen in digestive cancer: A systematic review and meta-analysis. European Journal of Surgical Oncology. 2018; 44: 1494-1503. doi: 10.1016/j.ejso.2018.07.052 DOI: https://doi.org/10.1016/j.ejso.2018.07.052
- Iwuji K, Almekdash H, Nugent K, Islam E, Hyde B, Kopel J, et al. Age-Adjusted D-Dimer in the Prediction of Pulmonary Embolism: Systematic Review and Meta-analysis. Journal of Primary Care & Community Health. 2021;12 (1): 1–8. doi: 10.1177/21501327211054996 DOI: https://doi.org/10.1177/21501327211054996
- Parpia S, Lapner S, Schutgen R, Elf J, Geersing G, Kearon C. Clinical pre-test probability adjusted versus age-adjusted D-dimer interpretation strategy for DVT diagnosis: A diagnostic individual patient data meta-analysis. J Thromb Haemost. 2020; 18: 669–675. doi: 10.1177/21501327211054996 DOI: https://doi.org/10.1111/jth.14718
- Yang M, Qi J, Tang Y, Wu D, Han Y. Increased D-dimer predicts the risk of cancer-associated recurrent venous thromboembolism and venous thromboembolism: A systematic review and meta-analysis. Thromb Res. 2020; 196: 410-413. doi: 10.1016/j.thromres.2020.09.031 DOI: https://doi.org/10.1016/j.thromres.2020.09.031
- Kumar V, Shaw J, Key N, Ilich A, Mallick R, Wells P, et al. D-Dimer Enhances Risk-Targeted Thromboprophylaxis in Ambulatory Patients with Cancer. The Oncologist. 2020; 25:1075–1083. doi: 10.1002/onco.13540 DOI: https://doi.org/10.1002/onco.13540
- Deng H-Y, Ma X-S, Zhou J, Wang R-L, Jiang R, Qiu X-M. High pretreatment D-dimer level is an independent unfavorable prognostic factor of small cell lung cancer. A systematic review and meta-analysis. Medicine. 2021; 100:15-22. doi: 10.1097/MD.0000000000025447 DOI: https://doi.org/10.1097/MD.0000000000025447
- Ma M, Cao R, Wang W, Wang B, Yang Y, Huang Y, et al. The D‑dimer level predicts the prognosis in patients with lung cancer: a systematic review and meta‑analysis. J Cardiothorac Surg. 2021; 16:243-254. doi: 10.1186/s13019-021-01618-4 DOI: https://doi.org/10.1186/s13019-021-01618-4
- Zhang C, Jia Y, Jia Y, Zhang X, Li K. Prognostic and predictive value of plasma d-dimer levels in patients with small-cell lung cancer. Int J Clin Oncol. 2018; 23 (6): 1070-1075. doi: 10.1007/s10147-018-1320-5 DOI: https://doi.org/10.1007/s10147-018-1320-5
- Ilich A, Kumar V, Henderson M, Mallick R, Wells P, Carrier M, et al. Biomarkers in cancer patients at risk for venous thromboembolism: data from the AVERT study. Thromb Res. 2020; 191: Suppl 1:S31-S36. doi: 10.1016/S0049-3848(20)30394-7 DOI: https://doi.org/10.1016/S0049-3848(20)30394-7
- Memon A, Sundquist K, PirouziFard M, Elf J, Strandberg K, Svensson P, et al. Identification of novel diagnostic biomarkers for deep venous thrombosis. Br J Haematol. 2018; 181 (3): 378-385. doi: 10.1111/bjh.15206 DOI: https://doi.org/10.1111/bjh.15206