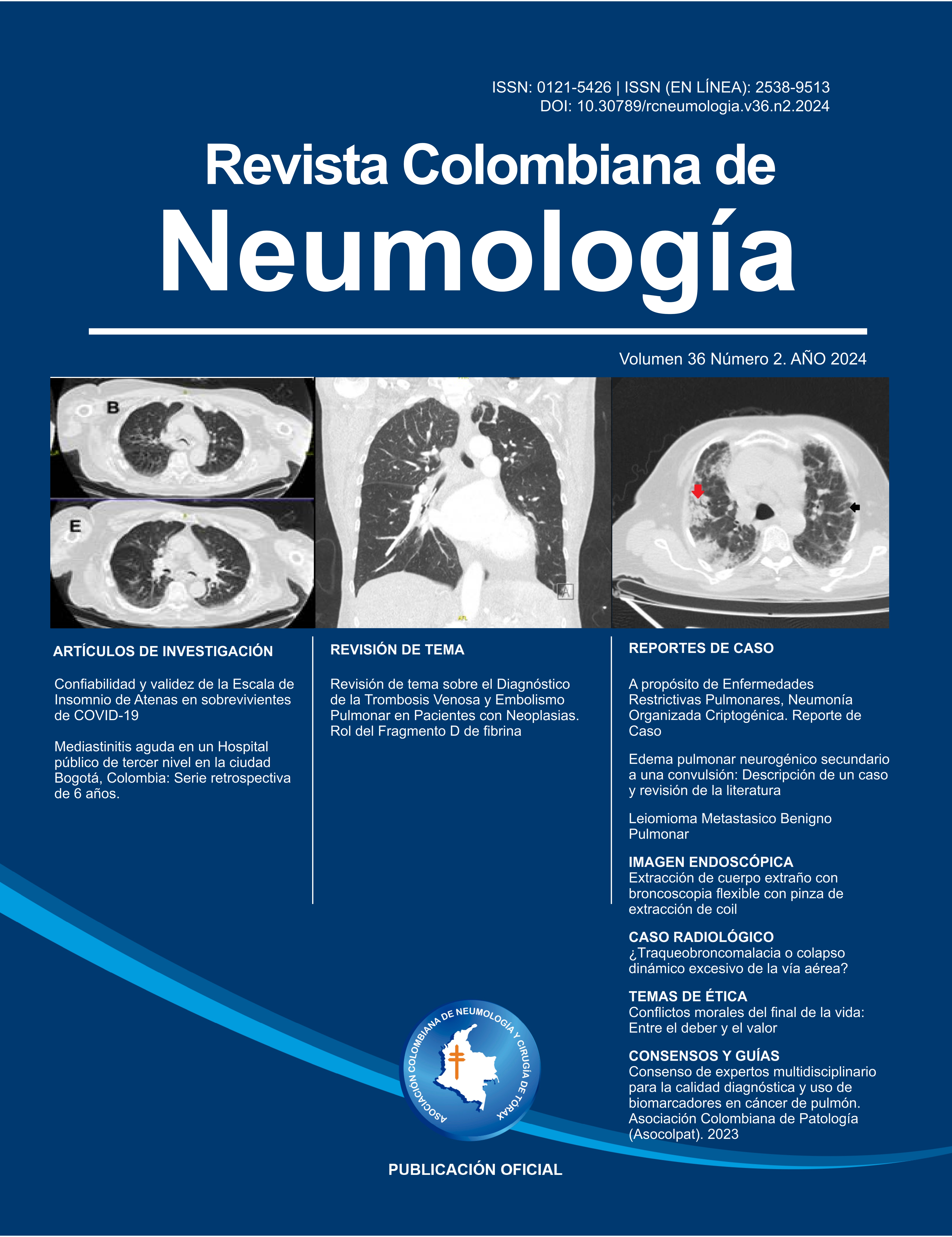
Confiabilidad y validez de la Escala de Insomnio de Atenas en personas recuperadas de la COVID-19
Reliability and validity of the Athens Insomnia Scale among Colombian People Recovered from COVID-19

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
Ninguna publicación, nacional o extranjera, podrá reproducir ni traducir sus artículos ni sus resúmenes sin previa autorización escrita del editor; sin embargo los usuarios pueden descargar la información contenida en ella, pero deben darle atribución o reconocimiento de propiedad intelectual, deben usarlo tal como está, sin derivación alguna.
Mostrar biografía de los autores
Introducción: La Escala de Insomnio de Atenas (EIA) es una herramienta con alta confiabilidad y validez para identificar casos de insomnio. Sin embargo, se desconoce el desempeño de la EIA en personas recuperadas de COVID-19. Objetivo: El estudio tuvo como objetivo probar la confiabilidad y validez de la EIA en una muestra colombiana de personas recuperadas de la COVID-19.
Material y Métodos: Trescientos treinta personas recuperadas de la COVID-19 completaron la EIA. Los participantes tenían entre 18 y 89 años (M = 47,7, ± 15,2) y el 61,5% eran mujeres. Se calcularon los análisis factoriales confirmatorios y el alfa de Cronbach.
Resultados: La EIA mostró aceptable estructura bidimensional. La primera dimensión (ítems 1 a 5, ‘problema de sueño nocturno’) presentó un alfa de Cronbach de 0,90, y la segunda dimensión (ítems 6 a 8, ‘disfunción diurna’) de 0,79.
Discusión y Conclusiones: La EIA presenta una estructura bidimensional, cada dimensión con alta consistencia interna, entre una muestra colombiana de personas recuperadas de la COVID-19. La EIA se puede utilizar para identificar casos de insomnio en personas recuperadas de COVID-19.
Visitas del artículo 1572 | Visitas PDF 647
Descargas
- Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2020;295:113599. doi: 10.1016/j.psychres.2020.113599 DOI: https://doi.org/10.1016/j.psychres.2020.113599
- Rogers JP, Chesney E, Oliver D, et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0 DOI: https://doi.org/10.1016/S2215-0366(20)30203-0
- Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4 DOI: https://doi.org/10.1016/S2215-0366(20)30462-4
- Chinvararak C, Chalder T. Prevalence of sleep disturbances in patients with long COVID assessed by standardised questionnaires and diagnostic criteria: A systematic review and meta-analysis. J Psychosom Res. 2023:175:111535. doi: 10.1016/j.jpsychores.2023.111535 DOI: https://doi.org/10.1016/j.jpsychores.2023.111535
- Soldatos C, Dikeos D, Paparrigopoulos T. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2020;48(6):555–560. doi: 10.1016/S0022-3999(00)00095-7 DOI: https://doi.org/10.1016/S0022-3999(00)00095-7
- Okajima I, Nakajima S, Kobayashi M, Inoue Y. Development and validation of the Japanese version of the Athens Insomnia Scale. Psychiatr Clin Neurosci. 2013;67(6):420–425. doi: doi.org/10.1111/pcn.12073
- Fornal-Pawłowska M, Wołyńczyk-Gmaj D, Szelenberger W. [Validation of the Polish version of the Athens Insomnia Scale]. Psychiatr Polsk. 2011;45(2):211–221.
- Gómez-Benito J, Ruiz C, Guilera G. A Spanish version of the Athens Insomnia Scale. Qual Life Res. 2011;20:931–937. doi: 10.1007/s11136-010-9827-x DOI: https://doi.org/10.1007/s11136-010-9827-x
- Jeong HS, Jeon Y, Ma J, et al. Validation of the Athens Insomnia Scale for screening insomnia in South Korean firefighters and rescue workers. Qual Life Res. 2015;24(10):2391–2395. doi: 10.1007/s11136-015-0986-7 DOI: https://doi.org/10.1007/s11136-015-0986-7
- Campo-Arias A, Monterrosa-Castro A, Herazo E, Monterrosa-Blanco A. Consistency and internal structure of the Athens Insomnia Scale in Colombian climacteric women. Eur Gynecol Obstet. 2020;2(2):123–126.
- Lin CY, Cheng AS, Nejati B, et al. A thorough psychometric comparison between Athens Insomnia Scale and Insomnia Severity Index among patients with advanced cancer. J Sleep Res. 2020;29:e12891. doi: 10.1111/jsr.12891 DOI: https://doi.org/10.1111/jsr.12891
- Sun JL, Chiou JF, Lin CC. Validation of the Taiwanese version of the Athens Insomnia Scale and assessment of insomnia in Taiwanese cancer patients. J Pain Sympt Manag. 2011;41(5):904–914. doi: 10.1016/j.jpainsymman.2010.07.021 DOI: https://doi.org/10.1016/j.jpainsymman.2010.07.021
- Keszei AP, Novak M, Streiner DL. Introduction to health measurement scales. J Psychosom Res. 2010;68(4):319–323. doi: 10.1016/j.jpsychores.2010.01.006 DOI: https://doi.org/10.1016/j.jpsychores.2010.01.006
- Chiu HY, Chang LY, Hsieh YJ, Tsai PS. A meta-analysis of diagnostic accuracy of three screening tools for insomnia. J Psychosom Res. 2016;87:85–92. doi: 10.1016/j.jpsychores.2016.06.010 DOI: https://doi.org/10.1016/j.jpsychores.2016.06.010
- Cronbach J. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16(3):297–334. doi: 10.1007/BF02310555 DOI: https://doi.org/10.1007/BF02310555
- StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015.
- World Medical Association. WMA Declaration of Helsinki – Ethical principles for medical research involving human subjects. Geneva: The World Medical Association; 2018.
- Bair L, Blais MA. Handbook of clinical scale in assessment in psychiatry and mental health. New York: Humana Press; 2010. DOI: https://doi.org/10.1007/978-1-59745-387-5
- Streiner D, Norman G. Health measurement scales: A practical guide to their development and use. 4th edition. Oxford: Oxford University Press; 2008.
- Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equat Model. 1999;6(1):1–55. doi: 10.1080/10705519909540118 DOI: https://doi.org/10.1080/10705519909540118
- Carmines EG, McIver JP. Analyzing models with unobservable variables. In: G Bohrnstedt, E Borgatta. Social measurement: Current issues. Beverly: Sage. 1981; pp. 65–115.
- Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129–1141. doi: 10.1016/S0140-6736(11)60750-2 DOI: https://doi.org/10.1016/S0140-6736(11)60750-2
- Morin CM, Drake CL, Harvey AG, et al. Insomnia disorder. Nat Rev Dis Primer. 2015;1(1):1–18. doi: 10.1038/nrdp.2015.26 DOI: https://doi.org/10.1038/nrdp.2015.26
- Atalay H. Insomnia: Recent developments in definition and treatment. Prim Care Community Psychiatry. 2006;11(2):81–91. doi: 10.1185/135525706X121138 DOI: https://doi.org/10.1185/135525706X121138
- Guandalini LS, da Silva EF, de Lima Lopes J, et al. Analysis of the evidence of related factors, associated conditions and at-risk populations of the NANDA-I nursing diagnosis insomnia. Int J Nurs Sci. 2020;7(4):466–476. doi: 10.1016/j.ijnss.2020.09.003 DOI: https://doi.org/10.1016/j.ijnss.2020.09.003
- Craven RF, Hirnle C, Henshaw C. Fundamentals of nursing: Concepts and competencies for practice. Philadelphia: Lippincott Williams & Wilkins; 2019.
- Faraklas I, Holt B, Tran S, Lin H, Saffle J, Cochran A. Impact of a nursing-driven sleep hygiene protocol on sleep quality. J Burn Care Res. 2013;34(2):249–254. doi: 10.1097/BCR.0b013e318283d175 DOI: https://doi.org/10.1097/BCR.0b013e318283d175
- Shang B, Yin H, Jia Y, et al. Nonpharmacological interventions to improve sleep in nursing home residents: A systematic review. Geriatr Nurs. 2019; 40(4):405–416. doi: 10.1016/j.gerinurse.2019.01.001 DOI: https://doi.org/10.1016/j.gerinurse.2019.01.001
- Coetzee JF. Evaluating diagnostic tests. South Afr J Anaesth Analg. 2004;10(5):7–16. doi: 10.1080/22201173.2004.10872376 DOI: https://doi.org/10.1080/22201173.2004.10872376
- Shapiro DE. The interpretation of diagnostic tests. Stat Meth Med Res. 1999;8(2):113–134. doi: 10.1177/096228029900800203 DOI: https://doi.org/10.1191/096228099666928387